What Are the Signs of Periodontal Disease?
What is Periodontal Disease?
1. Inflammation (Gingivitis)
Gingivitis is the inflammation of the gums. If you’re suffering from this condition, your gums will bleed whenever you brush or floss. In some cases, your teeth may lose their bright white- color.
Bacteria are always inside your mouth. They’re harmless unless certain conditions allow them to multiply drastically. It happens when you don’t do basic dental hygiene or go for a regular dentist visit.
2. Early Periodontal Disease
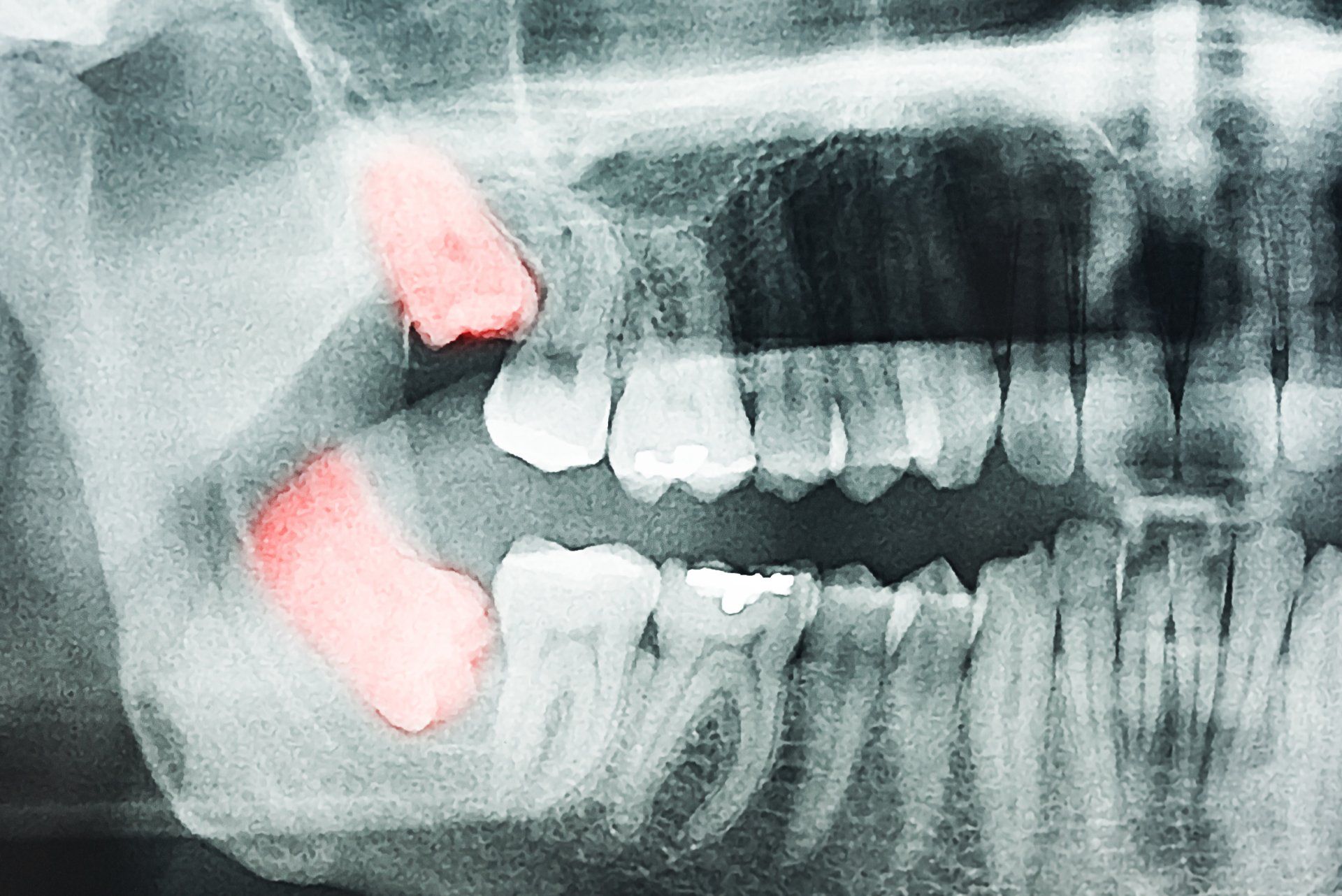
During its early stages, your gums will pull away from your teeth. Small pockets will form between your teeth and gums. These pockets serve as breeding grounds for harmful bacteria. As your immune system responds, it tries to stave off the infection. As with gingivitis, brushing and flossing will result in bleeding. You’ll also experience some bone loss during this period.
3. Moderate Periodontal Disease
After its initial stages, you'll now experience pain and bleeding around your teeth. Your gums will further recede. It causes your teeth to become loose since they won’t have enough bone support. The infection will cause your body to become inflamed. The inflammation goes beyond your mouth area at this point.
4. Advanced Periodontal Disease
Once you reach this phase, your teeth start falling off. The connective tissue holding them deteriorates. At the same time, the infection destroys your gums, bones, and other supportive tissues. Advanced periodontitis means experiencing severe pains while chewing. You may also get bad breath, and your mouth will always taste foul. Losing a few teeth is certain at this stage.
What Causes Periodontal Disease?
Risk Factors Affecting Periodontal Disease
Situations that lead to drastic hormonal changes put you at risk for periodontitis. The gum tissue becomes more sensitive during these situations. For example, entering puberty, menopause, menstrual cycles, or pregnancies raises your risk of inflammation. Some diseases also increase your chances of getting gingivitis. This includes diabetes, HIV, and cancer.
If you have a medical condition, you might take some medications. However, some side effects may increase your chances of getting gum diseases. When your medicine decreases your saliva flow, it will make you vulnerable to periodontal disease. Some examples include Dilantin and some brands of anti-angina medicine. These often cause your gum tissue to grow abnormally. Your age and family history also contribute to your gingivitis risks. If your parents have these diseases, you’re at risk. It comes from the bacteria type you get early on in life.
People with poor diet and lifestyle choices are at risk of gingivitis. If your daily menu lacks vitamin C, you’ll develop gum disorders. Regular smokers will experience gingivitis more.
Signs of Periodontal Disease
Red, Swollen Gums
These are some of the most common first signs of gum problems. In most cases, they start as inflammation along your gum line. They feel tender when touched. The swelling can get worse in time, causing your gums to bleed whenever you floss or brush.
Bad Breath
Your mouth’s environment provides a nice, warm, and moist home for millions of microbes. These creatures eat your plaque for sustenance and reproduction. The more you have, the faster they multiply. When they eat, bacteria will release toxins that irritate your gums. It causes you to have a foul mouth odor. It’s also a symptom of serious gum disorders since your breath won’t smell bad with gingivitis.
Receding Gums
If your teeth have a longer appearance than before, they may stop growing. This will make your gums start receding. As bones break, the gums make separate from the tooth, making a pocket.
Sensitive Teeth
Sipping a cold drink is nice during hot weather, but wincing at the pain can kill the mood.
Sensitive teeth are a definitive symptom of gum diseases. They occur at the same time as receding gums. When your gums shrink, it exposes the more sensitive part of your tooth, the dentin. It causes you to experience pain when drinking hot or cold water. You’ll also feel the pain when you leave your mouth open for long.
Wiggling or Shifting Teeth
Ask yourself whether your smile is consistent with your earlier pictures. If you notice something different, it might be a sign of gum disease. It attacks the bones holding your teeth together, loosening them. When your condition becomes too severe, the way you bite changes. Gum infections change how your teeth fit together. This often results in bite problems as time passes.
How Do Dentists Diagnose Periodontitis?
How to Treat Periodontitis
1. Good Oral Hygiene Practices
Once diagnosed, dentists will instruct you on how to decrease bacteria in your mouth. It involves methods that keep your teeth and gums clean. They’ll teach the proper toothbrush and flossing methods.
They will recommend oral hygiene products to complement your situation. In most cases, all you need is to brush your teeth twice each day. Use fluoride toothpaste to ensure you’re clean. If you have the budget, buy an electric toothbrush since it’s more effective. Floss every day to get rid of plaque. Never smoke or chew tobacco since it accelerates plaque growth.
2. Professional Cleaning
During this procedure, dentists will use tools and chemicals to remove plaque and tartar from teeth. They do it until the roots for a deeper level of cleaning. After that, they polish them before doing fluoride-based treatments.
For periodontal pockets, opt for deeper cleaning. Scaling and root planing helps remove tartar and rough spots on the tooth root. Expect bacterial levels to decrease a lot after these treatments.
3. Antibiotics
Sometimes, your dentist will prescribe antibiotics to help with hard-to-remove gum infections. It’s usually after professional cleaning failed to get rid of them. Depending on your preference, your antibiotic could be a tablet, capsule, gel, or mouthwash.
4. Follow-up Appointments
While treating gingivitis, your dentist will request follow-up sessions within the next few weeks. After that, your appointments will happen every three to six months. They will look into your progress.
If you still have periodontal pockets, they’ll likely prescribe other treatment procedures. In severe cases, surgery is the only option.
5. Surgery
Dentists recommend surgical treatments like flap surgery when the inflammation is in inaccessible mouth areas. These are places where you can’t brush or floss. This procedure cleans the deposits underneath your gums.
Flap surgery will place you in anesthesia. After that, they lift your gums away and clean the roots. They suture your gums back into place to finish the surgery.
When your periodontitis is bad enough, you’ll suffer from bone loss. In this situation, dentists recommend bone grafting procedures alongside flap surgery. It helps regenerate the lost bone mass.
Visit Your Dentist Now!